A pre-IUI workup for any couple being considered for IUI ought to include:
- Intensive clinical history of the two accomplices.
- Intensive actual assessment of the two accomplices.
- Semen test of male accomplice for semen investigations.
- Damage test to check for presence or nonappearance to
- hostile to sperm antibodies.
- Affirmation of ovulation in the female accomplice by:
- Follicular USG study.
- Day 21 P2 examine.
- Affirmation of tubal patency by:
- HSG
- Laparoscopic chromopertubation
- Hysterosalpingo-contrast-sonography (HyCoSy)
- Precluding uterine irregularities/cavity anomalies
Cautious determination of patients for IUI is a foundation for making progress rates. As an improper utilization of these medicines to the entire fruitless populace will cloud its adequacy, patient choice is vital IUI with Husband’s Semen-Indications: Careful determination of patients for IUI is a foundation for making progress rate. As an improper utilization of these medicines to the entire, the fruitless populace will cloud its adequacy, patient choice is vital IUI with Husband’s Semen-
Signs:
- Ejaculatory disappointment
- Cervical variable.
- Male Subfertility.
- Immunological
- Idiopathic barrenness
- Consolidated Infertility
- Physical imperfections
- Thick/frozen semen
- PCO
- HIV conflicting couple.
- Two-sided tubal square/tubal disease.
- Extreme pelvic provocative.
- Extreme oligoasthenoteratozoospermia.
- Loathe pelvic medical procedures or light.
According to the proposed rule for ART in India, an IUI focus has arrive at level 2 office which should have the framework for additional inside and out examination and progressed treatment of barrenness aside from where oocytes are taken care of outside the body. The IUI focus should have the accompanying offices:
For Investigation:
- Immunological test for barrenness.
- Sperm work test.
- Appraisal of TVS/follicular development
- Hysteroscopy/Laparoscopy/TV filter
Rundown of hardware:
- Laminar air unit
- Sperm counting chambers
- Microscopy
- Hatchery
- Rotator
Rundown of hardware:
- Laminar air unit
- Sperm counting chambers
- Microscopy
- Hatchery
- Rotator
Discretionary:
- Semen investigation
- Semen Freezer
- Semen Storage holder
- Hotter
Ovarian Stimulation
Follicular/ET observing
Seasons of Insemination
Ovarian Stimulation1. Ovarian Stimulation –
- Ovarian Stimulation –
- All can be performed either in an unstimulated normal cycle or in an invigorated cycle.
- There is proof that IUI with ovarian feeling bring about higher achievement rate than IUIonly
- The advantage of expanded pregnancy rate and live rate of birth accomplished with ovarian change should be adjusted against the observing and poetical entanglements like numerous pregnancies and ovarian hyperstimulation condition.
- Follicular/ET observing –
Observing the cycle is fundamental in the invigorated cycle to preclude the chance of OHSS/high request numerous pregnancies.
In the event that in excess of 4 mature follicles grow, most Infertility centers like to keep HCG infusion or leave the cycle or avoid intercourse, alternatively, the medicines cycle or medicines cycle can be switched over completely to Ivor GIFT as fitting.
Ultrasound checks thus do observing of follicular turn of events and endometrium regardless of blood chemicals test.
As the prevailing follicle comes to > 18 min distance across and endometrium is all around created HCG infusion is given to time insemination.
- Seasons of Insemination
- The exact timing of insemination is extremely tent to bring a higher achievement rate.
- IUI is done either when ovulation is up and coming or soon after.
- The strategy helps to time insemination in a characteristic cycle are:
- Ultrasound checks (Most solid).
- Detection of LH sugar in pee/blood (generally exact).
- Cervical bodily fluid appraisal (Not entirely solid)
- Basal internal heat level (Least exact)
Insemination is typically performed 24 to 48 hours after peeing LH sugar.
For animated cycles, insemination is normally performed around 40 hours after HCG infusion.
- Sperm washing and arrangement
Male accomplice produces semen by masturbation or frozen defrosted is utilized.
In instances of retrograde discharge, sperm is gathered from voided pee by centrifugation.
Just washed and arranged sperm are utilized for IUI in light of the fact that close to semen might cause a few uterine compressions/torments/squeezes and even breakdown at some point.
The point of washing and planning sperm:
- Separate sperm from planning sperm.
- Remove microbes, other trash, and synthetic that may contaminate and disturbance.
- To further develop sperm capacitation.
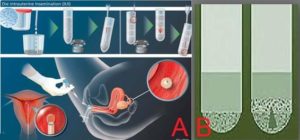
- Most common.
- Convenient method
- Separate good motile Sperms by allowing them to swim up to a large layer of sterile culture medium
- Procedure involves layering sterile culture medium over Liquefied semen.
- Sperm swim up into culture medium, Upper part of layered culture medium is removed and centrifuged and pellet is responded in a clean sterile medium.
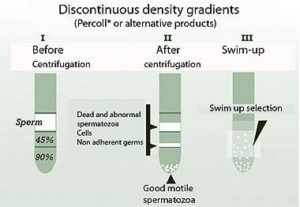
Density Gradient Technique:
- Separate normal Live sperm from seminal plasma and other cells and debris.
- Procedure Involves pipe ting semen sample on top a density gradient column ( a layer of fluid containing particles that act as filter) and then centrifuged
- Normal sperm becomes concentrated at the bottom of layer and can then be removed and washed by centrifugation and resuspenstion in clean medium.

Wash and Centrifugation
- The procedure involves diluting semen sample with a sterile culture medium and centrifuge. Following which the pellet is resuspended in culture medium and incubated.
- As per the Cochrane database there is no evidence that technology is superior to other although the trend suggest density gradient is the best.
- Presence of one million motile sperms after preparation seems to provide a realistic cutoff below which pregnancy rate are decreased.
- Morphology of sperm is also important and if the preparation of normal sperm falls below 4 present, pregnancy is rarely achieved.
- “Processed total motile sperm count correlate with pregnancy outcome after IUI” – Ohl DA, Miller DC, University of Michigan school of medicine.
- The result of the study has demonstrated that the PTMS count independently predicts success with IUI. Alternatives to IUI should be considered for the couple when PTMS count is less than 10 million.
The success rate of Insemination varies considerably between infertility clinics and insane clinic between different couples. Success rate between 5 to 30 present and depend on
many factors like:
- Cause of infertility.
- Endometriosis: Patient with severe endometriosis is not suitable for IUI because of meager success.
- Male factor infertility: Unstipulated IUI increases pregnancy rate by 2- fold.
- Stimulated IUI: Increase pregnancy rate by 5- fold.
- Unexplained infertility
- Tubal /ovulation factor
- Female parterre’s age
- Duration of infertility
- Sperm quality/ quantity
- Cycle rank
Complication of IUI:
- Failure of treatment.
- The possibility of using wrong semen sample.
- Infection/bleeding/trauma/Pain
- No infective salpingitis/allergic reactions
- Anti-sperm antibodies
- Multiple pregnancies
- Abortion/ectopic pregnancy
- OHSS
Indications for use of Donor Semen for IUI
- Severe oligo-/astheno-/teratozoospermia (in those not willing for IVF / ICSI)
- Azoospermia
- Genetic disorders
- These are now relative indications as the newer developments in the field of male infertility such as MESA/TESA/TESE male with opportunity for biological parenthood.
- Donor screening
- AIM:
- To prevent disease transmission
- To increase the chances of pregnancy by selecting appropriate semen parameters.
- Hence, complete medical and family history or complete physical examination/ appropriate investigations like blood group or typing, urine test, semen analysis (parameters to be judged as per WHO’s recent criteria) is important to rule out transmittable diseases, genetically inherited disorders.
- In case of attempted sperm banking, the sperm should be checked for good post-thaw recovers and prospective donors should be provided with relevant information and guidelines so that they understand moral/legal implications.
Instructions to Perspective Sperm Donor
- Not to supply more than 2 samples per week.
- Semen should be collected on site for it to be fresh at laboratory.
- They understand the moral/legal implications sample is allowed to liquefy at room temperature.
- The required volume of freezing medium in thawing.
- An equal volume of freezing medium is added and mixed slowly drop-wise.
- The mixture should be placed at 300C for 10 minutes.
- The tube is kept in the refrigerator at 40C for 90 minutes.
- Prepared sample is loaded into the cryovial.

- The cryovial is identified and removed from the goblet.
- Identification details on the removed cryovial are confirmed.
- Vials are placed in the water bath at 370C.
- Vials are swirled gently for 10 minutes.
- Complete liquefaction of the sample is confirmed.
- Contents are transferred into a round-bottomed tube.
- A quick count and motility study is performed.

- As per the study by Cleveland clinical center for advance research in human reproduction, the DI-SQ score (donor nsemination semen quality) Was an effective predictor of pregnancy and live birth outcomes in IUI patients who underwent AI with anonymous DISQ could also be used by sperm banks to help or select donors.
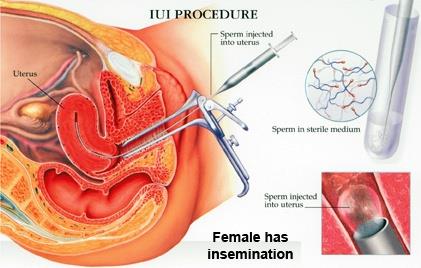
- Soon after identification of ovulation by TV scan assessment, male partner is instructed to collect semen.
- After collection semen sample is allowed to liquefy.
- Rapid semen analysis done to check count and motility.
- Sperm wash/preparation done by appropriate technique.
- Patient is given a good pre-procedure counseling about the procedure steps
- Patient is asked to void urine
- Placed on an examination table in dorsal or lithotomy position.
- It is preferable to elevate the foot end of the table.
- Physician should maintain asepsis throughout the procedure.
- Vulva and vagina cleaned with warm normal saline.
- Cuscos bivalved speculum is inserted into the vagina to expose the cervix.
- Vaginal discharge/cervical mucus should be cleaned with cotton swabs.
- Prepared and loaded sperm sample is checked for identity.
- Sperm loaded tuberculin syringe is attached to insemination cannula after removing air carefully.
- Loaded cannula is inserted into uterine cavity.
- Sperm gently pushed into the uterine cavity.
- Pushing air into the uterine cavity should be avoided .
- Cannula is removed after keeping it in position for 2 to 3 minutes. In foot end elevated position, patient is advised to rest for 10 to 15 minutes
1 DAY VS 2 DAY IUI TREATMENT CYCLES
Two day IUI treatment cycles are more successful than one day IUI cycles when using frozen thawed donor sperm – Matilsky, Geslevich Y, Haernek medical center, Israel. Such studies support the use of two day treatment cycles when using frozen thawed donor sperm while Cochrane database review does not support the difference in pregnancy rates with 1 day vs 2 day IUI treatment cycle especially with fresh semen samples.
With improved treatment options for HIV patients and the increase in their life expectancy, it is not surprising that many HIV patients desire to have children and discuss the available fertility options. Serodiscordant couples have limited options if they wish to have natural conception as sexual intercourse carries a risk of 1 in 500 times of transmitting the virus in semen to the female partner.
The only wholly safe option available to HIV discordant couples is adoption or in case of HIV positive males-sperm donation. Nevertheless, many couples desire genetically related offspring.
IUI forms one of the treatment options to serodiscordant couples willing for conception without seroconversion of uninfected partners.
In a serodiscordant couple, when female partner HIV positive IUI will suffice to prevent horizontal infection transmission. However, when the male partner is positive, sperm washing technique is used to minimize the infection of the healthy partner.
The absence of detectable HIV is verified before insemination using PCR-nucleic acid based sequence amplification assay.
Thus far, worldwide there are >3000 such cycles and 497 pregnancies with over 300 deliveries and no infection of the female partner or infant.
Pregnancy rate per insemination is 14% based on a European experience of more than 2000 insemination. Though current data from European programs suggest sperm washing to be a safety risk reduction option for heterosexual couples wishing to bear a child, CDC in the USA has recommended against insemination of women with semen from men infected from HIV.
“Safety of sperm washing and art outcome in HIV-1 serodiscordant couples”- Italian study in 2007 concluded sperm washing with a program of reproductive counseling was proved to be safe in a large series of 741 serodiscordant couples. The overall pregnancy rate of about 70.3% independent of the procedure used (IUI or IVF) justifies the effort of the medical team in setting up and implementing dedicated centers and individual patient in seeking a safe pregnancy.
